Big News! Greta Long, MA, LPC is Joining Summit Family Therapy
We are excited to welcome Greta Long, MA, LPC to the Summit Family Therapy team. Greta brings a warm, grounded presence and a thoughtful, relationship-centered approach to counseling that aligns deeply with our values of connection, collaboration, and meaningful change.
We are excited to welcome Greta Long, MA, LPC to the Summit Family Therapy team. Greta brings a warm, grounded presence and a thoughtful, relationship-centered approach to counseling that aligns deeply with our values of connection, collaboration, and meaningful change.
A Therapist Who Helps Clients Understand Themselves in Context
One of Greta’s greatest strengths is her ability to help clients make sense of their inner world within the context of their relationships. Our relationships—past and present—shape how we see ourselves, how we cope, and how we move through life. Greta helps clients slow down, reflect, and better understand these patterns so they can respond with intention rather than feeling stuck in cycles that no longer serve them.
Greta works from a person-centered, collaborative approach, meaning therapy is not something done to you—it is something built with you. Clients can expect a nonjudgmental, steady space where their experiences are honored and goals are shaped together. This approach is especially helpful for those who may feel anxious about starting therapy or who have struggled to feel fully understood in the past.
Supporting Life Transitions, Grief, and Relationship Challenges
Greta has a particular passion for working with individuals navigating life transitions, grief and loss, and relationship concerns. Whether someone is adjusting to a new season of life, processing the loss of a loved one, or trying to improve communication and boundaries in their relationships, Greta helps clients find clarity and emotional steadiness during uncertain times.
Clients often seek Greta’s support when:
Life feels overwhelming or uncertain
Grief or loss feels heavy or unresolved
Relationships feel strained or disconnected
Anxiety or stress increases during transitions
They want to better understand themselves and how they relate to others
Rather than rushing toward solutions, Greta helps clients understand why certain patterns exist—then gently supports them in creating healthier, more sustainable change.
A Calm, Grounding Presence in the Therapy Room
Beginning therapy can feel intimidating, and Greta is especially mindful of this. She is known for creating a calm, non-anxious environment where clients can take their time, ask questions, and feel supported from the very first session. Her style is steady, thoughtful, and compassionate—ideal for individuals who value reflection, emotional safety, and depth in the therapeutic process.
Using EMDR to Help the Brain Heal from Trauma and Distress
In addition to her relational, person‑centered approach, Greta incorporates Eye Movement Desensitization and Reprocessing (EMDR) into her clinical work when it is an appropriate fit for the client and their goals.
EMDR is an evidence‑based therapy that helps the brain reprocess distressing memories and experiences that can remain “stuck” in the nervous system. These experiences don’t have to be major, single‑event traumas—many people carry the emotional impact of chronic stress, relational wounds, grief, or past experiences that continue to shape how they feel, think, and respond today.
Rather than focusing only on talking through the past, EMDR helps clients:
Reduce the emotional intensity connected to painful memories
Shift long‑standing negative beliefs about themselves
Feel more grounded and present in daily life
Respond to triggers with greater flexibility and calm
Greta approaches EMDR with the same care and collaboration that defines her work overall. She prioritizes emotional safety, pacing, and preparation, ensuring clients feel supported and in control throughout the process. EMDR is always integrated thoughtfully—never rushed—and used alongside insight‑building and relational work to support lasting change.
This approach can be especially helpful for clients who feel they “understand” their struggles intellectually but still feel emotionally stuck, reactive, or overwhelmed despite their best efforts.
Education, Training, and Professional Background
Greta holds a Master’s degree in Counseling from Garrett-Evangelical Theological Seminary and is a Licensed Professional Counselor (LPC) in the state of Illinois. Her training integrates clinical skill with a deep respect for the whole person, allowing her to work effectively with clients from diverse backgrounds and life experiences.
Is Greta the Right Fit for You?
Greta may be an excellent fit if you are looking for a therapist who:
Values collaboration and mutual understanding
Helps you explore patterns in relationships and identity
Offers a steady, nonjudgmental presence
Supports both insight and practical growth
Honors your pace and your story
We are thrilled to have Greta as part of the Summit Family Therapy team and confident that her presence will be a meaningful resource for individuals and families in our community.
Now accepting new clients. We invite you to reach out and take the next step toward clarity, healing, and connection.
Codependency vs. Healthy Dependency: Understanding the Difference
In recent years, the term codependency has made its way into everyday language. It’s often used casually to describe “needy” behavior or intense attachment, but clinically, codependency is a complex relational pattern rooted in early experiences, trauma, and fears of abandonment. At the same time, humans are wired for healthy dependency — the mutual reliance that strengthens secure relationships.
In recent years, the term codependency has made its way into everyday language. It’s often used casually to describe “needy” behavior or intense attachment, but clinically, codependency is a complex relational pattern rooted in early experiences, trauma, and fears of abandonment. At the same time, humans are wired for healthy dependency — the mutual reliance that strengthens secure relationships.
One of the most important tasks in therapy is helping people distinguish between these two experiences. Understanding the difference is essential for building relationships that feel supportive, balanced, and emotionally safe.
What Is Codependency?
Codependency is commonly defined as a relational pattern in which one person becomes excessively emotionally or psychologically reliant on another—typically to the point of sacrificing their own needs, boundaries, or identity (Beattie, 1987; Cermak, 1986).
Key characteristics of codependency often include:
Difficulty saying no
Feeling responsible for others’ emotions or choices
Fear of abandonment or rejection
Self-worth tied to being needed
People‑pleasing to avoid conflict
Difficulty expressing personal needs
A pattern of choosing partners who are emotionally unavailable, unpredictable, or struggling with addiction
Cermak (1986) describes codependency as a “chronic pattern of dysfunctional caring,” where caretaking becomes compulsive and self-neglect becomes normalized.
In trauma‑informed terms:
Codependency often develops when early relationships required a child to be hyper-attuned to caregivers’ emotional states. In adulthood, this can transform into relationships driven by anxiety, over-functioning, or emotional enmeshment.
What Is Healthy Dependency?
Healthy dependency—also known as interdependence or secure dependence—is a natural, necessary part of human relationships.
Attachment science shows that humans are biologically wired for closeness, comfort, and co-regulation (Bowlby, 1988; Johnson, 2004). Healthy dependency is not weakness; it’s a sign of relational security.
Healthy dependency includes:
Mutual support and shared emotional labor
Freedom to express needs without fear
Balanced give-and-take
Maintaining individuality while staying connected
Respect for personal boundaries
Trust that the relationship can withstand honesty and conflict
Dr. Sue Johnson (2004), creator of Emotionally Focused Therapy, emphasizes that emotionally healthy adults “depend on each other without losing themselves.”
Codependency vs. Healthy Dependency: The Core Differences
1. Identity
Codependency: Sense of self becomes defined by caregiving, approval, or “being needed.”
Healthy Dependency: Both people maintain autonomy while staying emotionally connected.
2. Boundaries
Codependency: Blurred boundaries, difficulty saying no, fear that needs will push others away.
Healthy Dependency: Clear boundaries, comfort expressing limits and preferences.
3. Emotional Responsibility
Codependency: Feeling responsible for managing another person’s mood, choices, or reactions.
Healthy Dependency: Supportive but grounded—each person is responsible for their own emotional regulation.
4. Reciprocity
Codependency: One-sided giving, often driven by fear or obligation.
Healthy Dependency: Mutual responsiveness and shared emotional labor.
5. Motivation for Care
Codependency: Caregiving is tied to worthiness, fear of loss, or unresolved trauma patterns.
Healthy Dependency: Caregiving is grounded in love, respect, and authentic connection.
Why This Distinction Matters
When people confuse healthy dependency with codependency, they may:
Feel ashamed for having emotional needs
Avoid closeness to prevent “codependency”
Internalize the belief that needing others is a flaw
Over-correct by becoming hyper-independent
Hyper-independence can actually be a trauma response (Tummala‑Narra, 2007), not a sign of strength.
Recognizing the difference allows individuals to:
Build secure, emotionally safe relationships
Set healthier boundaries
Practice mutual vulnerability
Cultivate relational resilience
Moving Toward Healthy Dependency
Healing often involves shifting from fear-driven relating to connection grounded in security and self-worth. Some therapeutic steps include:
Identifying early attachment patterns
Practicing boundary-setting
Learning to tolerate uncomfortable emotions without over-functioning
Rebuilding self-worth separate from caretaking
Developing relationships with mutual emotional responsiveness
Therapy can be a powerful place to practice these skills and unlearn patterns that once felt necessary for survival.
Conclusion
Codependency is not simply “needing someone too much” — it is a pattern rooted in fear, trauma, and the belief that love is earned through self-sacrifice. Healthy dependency, on the other hand, is a sign of emotional maturity and secure attachment.
You are meant to lean on others. The goal is not to avoid dependency, but to practice it in ways that honor both your needs and your partner’s.
If you recognize codependent patterns in your own life, know this: healing is absolutely possible, and you are worthy of relationships built on safety, balance, and genuine connection.
References
Beattie, M. (1987). Codependent no more: How to stop controlling others and start caring for yourself. Hazelden.
Bowlby, J. (1988). A secure base: Parent-child attachment and healthy human development. Basic Books.
Cermak, T. L. (1986). Diagnosing and treating co-dependence. Alcoholism Treatment Quarterly, 4(1), 5–52.
Johnson, S. (2004). The practice of emotionally focused couple therapy: Creating connection. Brunner-Routledge.
Tummala‑Narra, P. (2007). Conceptualizing trauma and resilience across diverse contexts. Journal of Aggression, Maltreatment & Trauma, 14(1-2).
Understanding Trauma Bonds: What They Are—and What They Are Not
Trauma bonding is a term that has gained widespread attention in recent years, yet it is often misunderstood or misused in everyday language. In clinical and research contexts, a trauma bond has a specific meaning rooted in patterns of abuse, coercive control, and intermittent reinforcement. This article clarifies what a trauma bond truly is, what it is not, and why the distinction matters.
Trauma bonding is a term that has gained widespread attention in recent years, yet it is often misunderstood or misused in everyday language. In clinical and research contexts, a trauma bond has a specific meaning rooted in patterns of abuse, coercive control, and intermittent reinforcement. This article clarifies what a trauma bond truly is, what it is not, and why the distinction matters.
What Is a Trauma Bond?
An Emotional Bond Formed Within an Abusive Relationship
A trauma bond develops when a victim forms a powerful emotional attachment to an abuser through ongoing cycles of fear, threat, manipulation, and intermittent affection or relief. This dynamic creates a psychological trap that keeps the victim bonded to the perpetrator. According to foundational research by Dutton and Painter, trauma bonds emerge specifically from cyclical abuse and power imbalances.
Driven by Intermittent Reinforcement
The abuser alternates between cruelty and moments of kindness, apologies, or affection. This unpredictable “push‑pull” pattern strengthens attachment in ways similar to the behavioral mechanisms behind gambling rewards. Intermittent reward makes the victim cling tightly to the relationship, hoping for the “good” version of the abuser to return.
Occurs Across Many Forms of Interpersonal Violence
Trauma bonding is not exclusive to romantic partnerships. Research identifies trauma bonds in:
intimate partner violence
child abuse
incest
hostage situations
cults
human trafficking
hazing and high‑control group dynamics
Results in Loss of Agency and Self‑Concept
Victims in trauma bonds often internalize the abuser’s perception of them, losing a sense of autonomy and self‑worth. Over time, they may come to believe they cannot leave the relationship, or that they deserve the mistreatment.
Linked to Serious Mental Health Impacts
Long‑term consequences include:
low self‑esteem
depression
distorted self‑image
difficulty leaving abusive relationships
increased vulnerability to future partner violence
Not Simply a Victim Response—Sometimes It Is Strategically Engineered
Newer frameworks, such as weaponised attachment, emphasize how perpetrators deliberately groom, manipulate, and entangle victims to foster this bond before overt abuse begins—using love‑bombing, secrecy, and emotional dependency as tools of coercive control.
What a Trauma Bond Is Not
Not a Mutual Bond Formed Through Shared Pain or Trauma Disclosure
In casual conversation, some use “trauma bonding” to describe connecting with someone by sharing vulnerable or painful experiences. However, clinically, this is not trauma bonding. A trauma bond specifically involves abuse, not mutual storytelling or emotional intimacy.
Not Just a “Toxic” or Difficult Relationship
Many unhealthy relationships lack the core components of a trauma bond—particularly intermittent reinforcement, coercive control, and fear‑based attachment. Trauma bonding is more severe and systemic than everyday relational conflict or dysfunction.
Not a Sign of Weakness or Lack of Insight
Trauma bonds are neurobiologically reinforced survival strategies. Victims often stay because their nervous system is conditioned to seek safety from the same person causing harm. This is not a character flaw—it is a predictable outcome of the abuse cycle.
Not Explained by Attachment Alone
While attachment patterns may influence vulnerability, trauma bonding is distinct from anxious attachment or typical relational insecurity. A 2024 dissertation analyzing traumatic bonding profiles found that trauma bonds have unique features tied to power, self‑blame, punishment cycles, and coercive control, not just attachment dynamics.
Why the Distinction Matters
Misusing the term “trauma bond” can minimize the severity of abuse survivors' experiences or create confusion about what they are going through. Accurately identifying a trauma bond helps clinicians, survivors, and support networks understand:
why leaving an abusive relationship feels impossible
why the survivor may defend or idealize the abuser
how to structure trauma-informed interventions
how to restore autonomy and rebuild internal safety
Understanding what a trauma bond truly is gives survivors language for their experiences—and a roadmap toward healing.
References
Traumatic Bonding, Wikipedia: cyclical abuse, power imbalance, and contexts of trauma bonds.
Trauma Bonding, Psychology Today: definition, signs, and mechanisms of intermittent reinforcement.
Trauma Bonding and Interpersonal Violence, Reid et al. (2013): conceptualization and contexts of trauma bonding.
Palmer, M. (2024). An examination of how individuals experience a traumatic bond: latent profile analysis and distinctions from attachment.
When the Past Feels Present: How Epstein Files Coverage Can Shake Trauma Survivors—and How We Can Show Up for Each Other
The public release of the Epstein files has reopened a painful conversation about sexual exploitation, systemic failure, and the countless survivors who have endured these harms in silence. But alongside public outrage and political scrutiny, there’s a quieter, more intimate story unfolding—one happening inside the nervous systems of trauma survivors who are reliving echoes of their own experiences.
The public release of the Epstein files has reopened a painful conversation about sexual exploitation, systemic failure, and the countless survivors who have endured these harms in silence. But alongside public outrage and political scrutiny, there’s a quieter, more intimate story unfolding—one happening inside the nervous systems of trauma survivors who are reliving echoes of their own experiences.
If someone you love seems shaken, or if you feel unsettled and can’t quite explain why, you’re not alone. The emotional weight of stories like these can land hard, and understanding why they do is an important part of healing.
When the News Hits Too Close: Why the Epstein Files Impact Trauma Survivors So Deeply
For many survivors, the coverage surrounding the Epstein case is more than just news—it’s a reminder of harm that was ignored, minimized, or hidden. Psychiatrists have noted that survivors often face a “double jeopardy”: first the abuse, and then the disbelief or dismissal that follows, leaving wounds that can last for decades.
When the media revisits stories involving sexual exploitation, power imbalances, and failures to hold perpetrators accountable, survivors can feel retraumatized—especially when the disclosures include graphic details or emphasize how many warning signs were overlooked. Some of the recently released Epstein materials include sensitive descriptions of sexual assault, making them particularly triggering for individuals with a trauma history.
These reactions aren’t “overreactions.” They are nervous system responses shaped by lived experience and protective instinct.
What’s Happening in the Body: A Polyvagal Lens on Trauma Triggers
The physical and emotional reactions trauma survivors feel when exposed to triggering news stories can be better understood through polyvagal theory, developed by neuroscientist Stephen Porges. This framework explains how our autonomic nervous system responds to cues of safety or threat—often without conscious awareness.
The Three States of the Nervous System
Ventral Vagal State (Connection & Safety):
When the world feels safe, we can connect, think clearly, and regulate emotions.Sympathetic Activation (Fight or Flight):
When a story like the Epstein files hits the news, it can signal “danger,” leading to anxiety, agitation, or a sense of internal buzzing.Dorsal Vagal Shutdown (Freeze or Collapse):
When the threat feels overwhelming, survivors may emotionally shut down, disconnect, or feel numb—an autonomic strategy for self‑protection.
Polyvagal theory suggests that for trauma survivors, the nervous system can quickly shift into defensive states because earlier life experiences have “reconditioned” their internal alarms. What looks like an emotional reaction is, in reality, a physiological one.
Understanding this can help survivors meet their reactions with compassion—and help loved ones respond in more supportive ways.
How to Support a Friend or Loved One Who Is Triggered
When someone you care about is thrown off balance by traumatic news, your presence can make a meaningful difference. Here are ways to support them without overwhelming them:
Lead With Calm, Not Questions
Your tone of voice, facial expression, and pacing can cue their nervous system toward safety. This is called co-regulation, and it’s a powerful polyvagal-informed principle.
Validate Their Feelings
Sentences like:
“I’m here with you.”
“This makes sense.”
These can counter the invalidation many survivors have experienced—even decades after the trauma.
Invite (But Don’t Push) Grounding
Offer gentle options:
Slow breathing together
Looking around the room
Feeling feet on the floor
These help re-engage ventral vagal pathways that support emotional regulation.
Protect Their Peace
Encourage stepping back from the relentless news cycle. The Epstein materials are extensive and, in some cases, graphic; boundaries around media exposure can be essential for nervous system stability.
Ask What Support Looks Like
Let them define what they need. Trauma often involves a loss of agency; offering choice helps restore it.
How Therapy Can Help Survivors Navigate Triggers and Heal
Therapy—especially trauma informed approaches grounded in polyvagal theory—can help survivors understand their nervous system, regain emotional flexibility, and restore a sense of safety in their bodies and relationships.
Polyvagal-informed therapies focus on:
Recognizing and mapping autonomic states
Identifying triggers and cues of safety
Strengthening vagal regulation through breath, movement, vocalization, and relational connection
Building resilience through co-regulation with a therapist
These modalities help survivors shift from being “stuck” in survival states to experiencing more moments of ventral vagal calm and connection. Research shows that polyvagal-informed approaches enhance emotional regulation and reduce trauma symptoms.
Therapy also provides a space to process the secondary trauma that news coverage like the Epstein files can stir—the anger, the grief, the sense of systemic betrayal—and to reconnect with hope.
References
Moffic, H. S. (2025). The Epstein Files, the Abuse of Women, and Psychiatry. Psychiatric Times.
Institute for Functional Medicine. (2024). Understanding PTSD From a Polyvagal Perspective.
PBS News. (2026). The latest Epstein files release includes famous names and new details about an earlier investigation.
U.S. Department of Justice. (2026). Epstein Library (Epstein Files Transparency Act Disclosures).
Sky News. (2026). Epstein files: The key findings so far.
Psychotraumatology Institute. (2025). Polyvagal Theory–Informed Therapies.
Navigating Grief Together: A Message from Dr. Courtney Stivers
Over the past two weeks, our workplace community has been touched by a profound wave of loss. Three of our employees have experienced the passing of close loved ones, and within my own extended family, we are mourning the loss of a child to cancer. These moments remind us of the fragility of life, the depth of human love, and the universal experience of grief that connects us all.
Over the past two weeks, our workplace community has been touched by a profound wave of loss. Three of our employees have experienced the passing of close loved ones, and within my own extended family, we are mourning the loss of a child to cancer. These moments remind us of the fragility of life, the depth of human love, and the universal experience of grief that connects us all.
Grief is not a linear journey, nor is it something that follows rules or timelines. It arrives without warning, lingers in unexpected ways, and reshapes our understanding of the world. For some, it shows up as tears. For others, silence. For many, it appears as exhaustion, confusion, or even moments of laughter that bring guilt. All these experiences are real, valid, and deeply human.
The Weight We Carry
When loss touches a workplace, it doesn’t stay at the door. We bring our whole selves to our work—our strengths, our fears, our hopes, and our heartaches. As we navigate these recent losses, it's important to recognize that grief affects each of us differently. There is no “right way” to mourn. What matters is that no one faces it alone.
To everyone else who wants to help: your compassion and patience can be a powerful source of comfort. Sometimes the smallest gestures—checking in, offering help, or simply acknowledging someone’s pain—can mean more than you realize.
When Grief Hits Close to Home
As I walk through grief within my own family, I am reminded of both the pain and the privilege of being human. Losing a child—especially to something as senseless as cancer—is a wound that words cannot fully hold. My family is learning, day by day, how to breathe differently, love differently, and find meaning again in the midst of heartbreak.
Sharing this with you is not easy, but it feels important. Leaders are not immune to loss. Professionals do not cease to be vulnerable. And even those who help others through their darkest moments must also learn to walk through their own.
Years ago, I endured the painful loss of my mother after her battle with an aggressive from of breast cancer. Losing a parent leaves a particular kind of void—one filled with memories, gratitude, and the ache of unfinished conversations.
During that time, my family was lifted by tremendous support from friends, loved ones, and our community. Their meals, prayers, messages, and simple presence reminded us that even in the darkest seasons, we do not walk alone. That support helped shape how I understand compassion today—and it continually inspires the way I show up for others in moments of loss.
Supporting One Another Through the Process
Grief becomes more bearable when it is met with community. In the coming days and weeks, I encourage all of us to:
Show grace — to yourself and others.
Lean on the support available — whether through colleagues, friends, mental health resources, or spiritual practices.
Recognize signs of overwhelm — such as withdrawal, irritability, or fatigue — and reach out when you notice them in others.
Allow yourself to feel — whatever arises, without judgment.
Healing doesn’t mean forgetting. It means finding ways to carry our memories forward while learning to live with a new kind of normal.
Sending hugs to anyone who is hurting today. You do not have to go through it alone.
Meet Our New Clinical Director of Family Services!
We are delighted to share an exciting milestone in the growth of our practice. Kate Mills, MA, LCPC has been promoted to Clinical Director of Family Services at Summit Family Therapy!
For years, Kate has been a cornerstone of what makes Summit special. Her dedication, compassion, and professionalism have profoundly shaped the experiences of our clients and our team. This promotion reflects not only her clinical expertise, but also the exceptional heart, leadership, and integrity she brings into every room she enters.
Dear Friends, Clients, and Community Partners,
For years, Kate has been a cornerstone of what makes Summit special. Her dedication, compassion, and professionalism have profoundly shaped the experiences of our clients and our team. This promotion reflects not only her clinical expertise, but also the exceptional heart, leadership, and integrity she brings into every room she enters.
A Leader Who Embodies Our Values
Kate is known for her deep respect for each individual’s story and her unwavering belief that every person deserves to be heard. She has helped cultivate a workplace where empathy, authenticity, and collaboration flourish—values that radiate into the care our clients receive every day.
Her work ethic and commitment to excellence set a high standard for our entire team. Whether supporting colleagues, consulting on cases, or introducing innovative therapeutic ideas, Kate consistently leads with calm confidence, example, and an encouraging spirit.
Advanced Training & Specializations
Kate’s clinical expertise is both broad and highly specialized. Her flexible, person-centered approach incorporates talk therapy, cognitive-behavioral strategies, EMDR, expressive arts, and play—ensuring that every client can find a path to healing that feels safe, meaningful, and empowering.
A Heart for Families & Community
Kate has a natural gift for helping clients discover deeper meaning and connection within themselves and their relationships. Her warmth and insight have guided countless individuals and families toward resilience, peace, and healthier ways of living.
Outside the therapy room, Kate’s joyful, grounded presence continues to inspire. She draws strength from her large extended family, and she cherishes time spent with her three sons and their dogs—whether playing games, exploring outdoors, or enjoying a great TV re-run or new food adventure.
We are thrilled for what this next chapter means not only for Kate, but for our entire Summit Family Therapy community. Her leadership will continue to shape our commitment to providing compassionate, evidence-based care for individuals, couples, and families across all seasons of life.
Please join us in celebrating Kate Mills!
We are grateful to have her guiding our mission and strengthening the work we do every day.
Warmly,
The Summit Family Therapy Team
When Friendship Feels Hard: Understanding the Barriers That Keep Us Apart
Most of us agree that friendship is important, yet many people quietly struggle to create and maintain meaningful relationships. As a therapist, I hear this often:
“I’m terrible at making friends.”
“Everyone else seems to have a social circle. What's wrong with me?”
“My friendships drift as life gets busier.”
“I don’t even know where to start.”
Most of us agree that friendship is important, yet many people quietly struggle to create and maintain meaningful relationships. As a therapist, I hear this often:
“I’m terrible at making friends.”
“Everyone else seems to have a social circle. What's wrong with me?”
“My friendships drift as life gets busier.”
“I don’t even know where to start.”
If you’ve ever felt this way, you’re not alone. There are very real, very human reasons people find friendship harder in adulthood.
Let’s talk about some barriers and why investing in relationships is still one of the best things you can do for your well-being. (See my previous post for more information on how friendships impact our health).
Barrier 1: We’re Busy. Really Busy
Between work, family duties, childcare, and the daily logistics of life, many adults simply run out of time and emotional energy. Friendship often becomes the thing we get to “when life slows down,” except life rarely does.
Potential Solution:
Schedule connection the same way you schedule appointments. Friendship deserves a place on the calendar.
Barrier 2: Life Transitions Change Our Social World
Moves, breakups, new jobs, parenthood, health challenges or other transitions reshape our routines and priorities. Even strong friendships can weaken without intentional effort.
Potential Solution:
Acknowledge that friendships naturally ebb and flow. Reach out even when years have passed. Reconnection is often easier than we fear.
Barrier 3: We Rely Too Heavily on Digital Connection
Social media can trick us into feeling “connected” while offering little of the emotional engagement that real friendship provides. Online interactions often lack depth, vulnerability, and mutual support.
Potential Solution:
Supplement digital contact with real conversations when possible. Challenge yourself to use voice notes, phone calls, or in-person time.
Barrier 4: We Learn Early to Prioritize Self-Sufficiency
Many people internalize the belief that needing others is a sign of weakness. But emotionally healthy people do lean on each other: not because they’re fragile, but because connection is part of being human.
Potential Solution:
Try reframing reaching out as strength: “I value this relationship enough to invest in it.”
Barrier 5: Fear of Vulnerability
To form a close friendship, we need to let people see the real us; our hopes, fears, insecurities. That can feel risky, especially if we’ve been hurt before.
Potential Solution:
Start small. Share honest pieces of yourself gradually, giving others the opportunity to know you a little at a time. Trust is built, not assumed.
Friendships Are Worth the Effort
Even with these challenges, research consistently shows that meaningful friendships improve mental health, increase resilience, and create a buffer against life’s stressors.
Friendship is not effortless. But like any worthwhile investment, the rewards far outweigh the work.
Further Reading & Resources
If you’d like to explore this topic further, these resources offer research-based insight in a way that’s approachable, validating, and practical. You don’t need to read or watch everything, consider choosing what feels most relevant to where you are right now.
Books
Platonic: How the Science of Attachment Can Help You Make—and Keep—Friends by Marisa G. Franco Ph.D.
Helpful if you: struggle with initiating friendships, feel unsure how to deepen connections, or wonder why friendship feels harder as an adult.Friendship: The Evolution, Biology, and Extraordinary Power of Life’s Fundamental Bond by Lydia Denworth
Helpful if you: like understanding the “why” behind human behavior and want reassurance that friendship truly matters for mental and physical health.Attached.: The New Science of Adult Attachment and How it can Help You Find - and Keep - Love by Amir Levine, M.D. and Rachel S.F. Heller, MA
Helpful if you: Want to read about how attachment patterns influence adult relationships, not just romantic onesTogether: The Healing Power of Human Connection in a Sometimes Lonely World” by Vivek H. Murthy, MD
Helpful if you: Want to explore loneliness as a public health issue and the role of meaningful relationships
The Fourth “F” — Fawning
Most people are familiar with the classic trauma responses: fight, flight, and freeze. But trauma research has increasingly recognized a fourth response that often hides in plain sight: fawning.
Most people are familiar with the classic trauma responses: fight, flight, and freeze. But trauma research has increasingly recognized a fourth response that often hides in plain sight: fawning.
In her book Fawning: Why the Need to Please Makes Us Lose Ourselves — and How to Find Our Way Back, psychologist Dr. Ingrid Clayton describes fawning as a hybrid trauma adaptation—a subconscious survival strategy in which a person moves toward the source of threat rather than away from it. Instead of protecting ourselves through avoidance or defense, we attempt to secure safety by appeasing, pleasing, or over‑accommodating the person who feels unsafe or unpredictable.
What Fawning Is (and Isn’t)
Fawning is often mistaken for people‑pleasing or codependency, but the underlying motivation is different.
People‑pleasing is typically about wanting to be liked.
Codependency involves enmeshment and lack of boundaries.
Fawning, however, is a trauma‑based response rooted in fear, insecurity, and the need for emotional or physical safety.
Fawning shows up when we feel inexplicably drawn closer to someone who causes harm or instability—something that doesn’t make logical sense but makes emotional survival sense. Instead of withdrawing from pain or dysfunction, we move toward it, hoping to minimize conflict or avoid abandonment.
Why Fawning Keeps Us Stuck
Fawning helps explain why people:
Stay in harmful relationships
Remain in toxic workplaces
Tolerate dysfunctional environments
Ignore red flags that seem obvious to others
Like all trauma responses, fawning originally served a purpose—it helped someone survive an unsafe environment. But when it becomes an automatic, lifelong pattern, it can lead to resentment, burnout, loss of identity, and chronic self‑silencing.
Signs You Might Be “Fawning”
If you’ve ever found yourself doing the following, you may be operating from a fawn response:
Apologizing to someone who hurt you in an attempt to defuse tension
Ignoring a partner’s harmful behavior because speaking up feels dangerous
Staying up late or overworking to stay on your boss’s “good side”
Befriending bullies or difficult people to reduce conflict
Worrying constantly about saying the “wrong” thing
Shifting your personality, preferences, or opinions for approval
At its core, fawning is about earning safety through compliance—a strategy that may once have been protective but becomes harmful when it replaces healthy boundaries.
How Therapy Helps Break the Fawn Response
Healing requires learning new ways to experience safety, connection, and self‑expression. Several evidence‑based therapies can support this process:
Cognitive Behavioral Therapy (CBT): Helps identify survival‑based beliefs (“I’m only safe if everyone is happy with me”) and replace them with healthier cognitions.
Dialectical Behavior Therapy (DBT): Strengthens emotional regulation, boundary‑setting, and distress tolerance.
Internal Family Systems (IFS): Helps explore protective parts of the self that developed the fawn response.
Eye Movement Desensitization and Reprocessing (EMDR): Reprocesses traumatic memories that created the pattern.
Somatic Experiencing: Helps the nervous system learn safety through body‑based awareness and regulation.
Fawning is not a character flaw—it’s a trauma imprint. With the right support, people can reconnect with their authentic selves, develop healthy relationships, and rebuild a sense of internal safety.
References
Clayton, I. (2023). Fawning: Why the need to please makes us lose ourselves—and how to find our way back.
Herman, J. L. (2015). Trauma and recovery: The aftermath of violence—from domestic abuse to political terror. Basic Books.
Linehan, M. M. (2015). DBT skills training manual (2nd ed.). Guilford Press.
Porges, S. W. (2011). The polyvagal theory: Neurophysiological foundations of emotions, attachment, communication, and self-regulation. W. W. Norton.
Schwartz, R. C. (2021). No bad parts: Healing trauma and restoring wholeness with the internal family systems model. Sounds True.
Shapiro, F. (2018). Eye movement desensitization and reprocessing (EMDR) therapy (3rd ed.): Basic principles, protocols, and procedures. Guilford Press.
van der Kolk, B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. Viking.
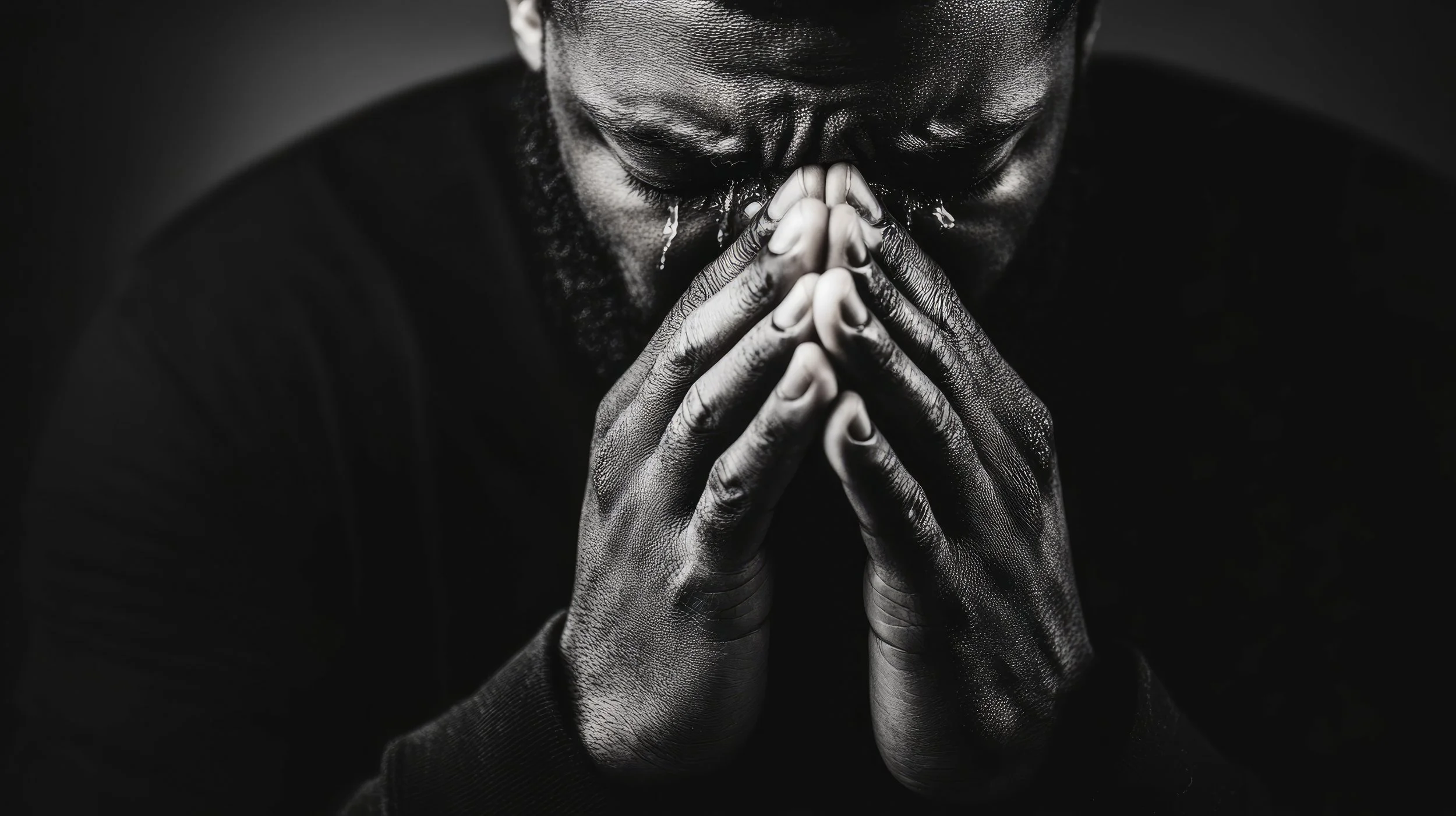
The Silent Weight Men Carry
“Suck it up, butter cup.”
“Rub some dirt in it.”
Most men have heard some version of these lines, little slogans wrapped in toughness and handed to boys long before they ever understand what they mean. Years ago, someone said I was “the least masculine employee.” To this day, I still don’t know what that’s supposed to mean.
“Suck it up, butter cup.”
“Rub some dirt in it.”
Most men have heard some version of these lines, little slogans wrapped in toughness and handed to boys long before they ever understand what they mean. Years ago, someone said I was “the least masculine employee.” To this day, I still don’t know what that’s supposed to mean.
Some men reading this may already be rolling their eyes or getting ready to accuse me of being woke. But stay with me, because what I’m talking about isn’t politics. It’s pain. It’s shame. It’s the quiet, suffocating struggle that too many men carry alone.
The Shame That Chokes
The shame men feel about seeking mental health support in our culture is palpable. In fact, it’s choking the life out of men who desperately need help but don’t feel allowed to ask for it. We’ve placed this bizarre expectation on men to “have it all together,” as if being male somehow comes with a manual for emotional invincibility.
Understanding the origins of these cultural expectations is important, but that’s a paper for another day. Today, I want to speak from the heart and from years of working with men from every walk of life.
The High Cost of Silence
I’ve worked with hundreds of men and boys, and nearly all of them have struggled under the same pressure:
Be strong.
Don’t cry.
Hold it together.
Don’t let them see you sweat.
I see this pressure at its most intense in first‑responder and military communities. These men are expected to have the answers, rise to the occasion, and if necessary, even meet violence with violence. But ask them how they’re feeling? Suggest that they practice self‑care or see a therapist? Some would rather walk it off even if they’re metaphorically (or literally) bleeding out.
Think Monty Python’s “It’s only a flesh wound” scene from the Holy Grail. That’s how a lot of men treat emotional injuries, as if admitting harm is worse than the harm itself.
Even in faith settings, men are expected to be unwavering pillars, protectors, providers, and leaders. But what happens when they fall short? When they doubt, struggle, or crumble under expectations?
Shame swoops in.
Shame tells them they’re less than other men.
Not good enough.
Not strong enough.
Not smart enough.
Not spiritual enough.
And men begin comparing themselves to other men, it’s what we do, usually while everyone is pretending they’re fine making small talk about the latest game or trend.
So, What Should Men Do?
If you’re a man reading this, here’s a hard but honest question:
Do you know how your behavior and your words impact the people around you?
Sometimes the expectations we cling to, the ones we think make us men, are the very things holding us back from real connection, growth, and emotional depth. It’s possible that what you were taught to value is actually harming your relationships and your own development.
So, here’s the real test of courage:
Can you admit you need help?
Can you take the first vulnerable step toward change?
Because being a man has nothing to do with being the strongest or the most dominant person in the room. It’s about how you show up.
Do people feel secure around you?
Do you act with integrity?
Do your values line up with your behavior?
These are the real markers of strength.
A New Kind of Masculinity
Men deserve deeper connections, richer relationships, and the freedom to be fully human, and not just stoic warriors marching silently toward burnout or breakdown.
If you’ve ever felt like you needed to “suck it up,” maybe today is the day you don’t.
Maybe today is the day you loosen your grip and admit:
“This is heavy, and I can’t carry it alone.”
Because asking for help doesn’t make you weak.
It makes you honest.
It makes you courageous.
And most importantly, it makes you whole.
Hat, Haircut, and Tattoo Decisions: A Better Way to Decide Almost Anything
Years ago, I stood in a store holding a sweater I didn’t need but really liked.
It wasn’t expensive. It wouldn’t change my life. And yet, I stood there debating it like I was deciding whether to quit my job.
At the same time, I was doing the opposite in other areas of my life. I tended to make impulsive, rushed, high-stakes decisions with far less thought than they deserved.
Years ago, I stood in a store holding a sweater I didn’t need but really liked.
It wasn’t expensive. It wouldn’t change my life. And yet, I stood there debating it like I was deciding whether to quit my job.
At the same time, I was doing the opposite in other areas of my life. I tended to make impulsive, rushed, high-stakes decisions with far less thought than they deserved.
I was reminded of this dilemma when presented with the mental model James Clear shares in Atomic Habits: hat, haircut, and tattoo decisions (Clear, 2018).
Once I learned it, I started noticing how often I get decision-making backwards.
The Mental Model
James Clear breaks decisions into three categories:
Hat decisions are easy to reverse. You try them on. If you don’t like them, you take them off.
Haircut decisions take time to undo. You’ll live with the result for a while, but it’s not permanent.
Tattoo decisions are long-lasting or irreversible. They shape your identity and future options.
The issue isn’t poor judgment.
It’s misclassifying the decision.
Hat Decisions: Low Risk, High Learning
Buying the sweater was a hat decision.
The downside was limited. The upside was learning whether I’d actually enjoy wearing it. Either way, the cost of being wrong was small.
Hat decisions tend to be:
Low cost
Reversible
Rich in feedback
And yet, these are the decisions we overthink the most.
We hesitate to:
Try a new routine
Publish a piece of writing
Attend one class or event
Test a new tool or habit
Behavioral science consistently shows that small experiments reduce fear and increase action. This is the foundation of Eric Ries’ Lean Startup methodology, which emphasizes rapid experimentation and learning over premature optimization (Ries, 2011).
Psychologically, this works because it lowers perceived risk and bypasses loss aversion: the tendency to overweight potential losses relative to gains (Kahneman & Tversky, 1979).
Hat decisions aren’t about being right.
They’re about learning quickly.
Haircut Decisions: Commit, Then Revisit
Changing jobs, on the other hand, is not a hat decision.
It’s a haircut.
When I changed roles a few years ago, I knew I wasn’t locking myself into a permanent identity; but I also knew the decision would shape my skills, network, and trajectory for years. There were switching costs. I couldn’t just undo it next week.
Haircut decisions:
Require commitment
Have delayed feedback
Are reversible, but not instantly
Examples include:
Changing roles or career direction
Moving to a new city
Taking on a long-term project
Committing to a serious fitness or financial plan
Research on goal-setting shows that commitment paired with clear review points leads to better outcomes than either indecision or blind persistence (Locke & Latham, 2002).
Instead of asking, “Is this perfect?”
A better question is:
“Can I commit to this for a defined period and reassess honestly?”
Haircut decisions shouldn’t trap you, but they should be taken seriously.
Tattoo Decisions: Slow Down and Zoom Out
Then there are tattoo decisions.
For me, this looked like making a meaningful financial sacrifice early in my career: choosing flexibility and alignment over immediate compensation. That choice closed some doors while opening others.
Tattoo decisions tend to:
Be difficult or impossible to reverse
Shape identity
Influence future options in compounding ways
Examples include:
Marriage
Having children
Starting a company
Taking on significant debt
Publicly anchoring your identity to a role or belief
James Clear emphasizes that identity-based decisions are the hardest to undo, because once something becomes part of who we think we are, it reinforces future behavior (Clear, Identity-Based Habits).
This is why tattoo decisions deserve slowness: not fear, but reflection.
Tattoo decisions aren’t about efficiency.
They’re about alignment.
The Hidden Cost of Category Errors
Most decision-related stress comes from treating the wrong decisions as permanent.
Overthinking hat decisions leads to anxiety and stagnation
Rushing tattoo decisions leads to regret
Cognitive biases help explain why:
Loss aversion magnifies small risks
Social evaluation inflates trivial choices
Present bias downplays long-term consequences (Thaler, 1981)
Clarity returns when you ask:
What kind of decision is this, really?
A Simple Filter
When faced with a difficult choice, ask:
How reversible is this?
What’s the worst (realistic) downside?
What information will I gain by acting?
Then match your speed accordingly:
Hat → act quickly
Haircut → commit with a timeline
Tattoo → slow down and zoom out
Why This Matters for Habits and Growth
Most meaningful change doesn’t begin with a tattoo decision.
It begins with hat decisions repeated consistently.
Research on self-perception theory suggests that we infer identity from behavior, not intention (Bem, 1972). Small actions, repeated over time, quietly reshape how we see ourselves.
By lowering the stakes on most decisions, we make better ones on the few that truly matter.
So buy the sweater - or don’t - but don’t let it drain your energy.
Save that care for the decisions that will still matter years from now.
Does this idea resonate with you? Check out my works cited, or here's a short list of recommendations:
Atomic Habits by James Clear
The foundation. Clear’s work on identity-based habits explains why small, reversible actions compound into permanent change, and where the hat, haircut, tattoo framework fits into a bigger picture.
https://jamesclear.com/atomic-habitsIdentity-Based Habits (Article) by James Clear
A short, high-impact read that clarifies why some decisions feel permanent: once something becomes part of your identity, it’s much harder to undo.
https://jamesclear.com/identity-based-habitsThinking, Fast and Slow by Daniel Kahneman
A classic on how humans misjudge risk and consequence. Especially useful for understanding why we overthink low-stakes decisions and underestimate long-term ones.Hat, Haircut, Tattoo Decisions (Video)
A clear, accessible breakdown of the framework in video form. Great if you want a quick refresher or prefer visual explanations.
https://www.youtube.com/watch?v=AHIXRo7zICM
The Grieving Body: How Loss Lives in the Body
Grief is one of the most painful and disorienting human experiences. Many describe it as feeling as though a part of themselves has been cut away—an absence so profound it is felt not only emotionally, but physically. In The Grieving Brain, psychologist and neuroscientist Mary‑Frances O’Connor, PhD, offers compelling scientific and clinical insight into why grief feels the way it does and how loss fundamentally reshapes the body and brain.
A Book Review of The Grieving Body By Mary‑Frances O’Connor, PhD.
Grief is one of the most painful and disorienting human experiences. Many describe it as feeling as though a part of themselves has been cut away—an absence so profound it is felt not only emotionally, but physically. In The Grieving Brain, psychologist and neuroscientist Mary‑Frances O’Connor, PhD, offers compelling scientific and clinical insight into why grief feels the way it does and how loss fundamentally reshapes the body and brain.
O’Connor’s work challenges the common misconception that grief is “all in our head.” Instead, she demonstrates that grief is a whole‑body experience, rooted in biology, attachment, and survival.
Grief as a Biological Experience
According to O’Connor, bereavement activates powerful physiological responses. The death of a loved one can trigger increased heart rate, elevated blood pressure, heightened stress hormones, and inflammatory processes throughout the body. These responses occur because close relationships are not simply emotional bonds—they are part of our survival system.
Humans are wired for attachment. When we form a close bond, our nervous systems become attuned to another person’s presence, habits, and rhythms. Over time, the brain comes to rely on that relationship in ways that operate largely outside of conscious awareness. The sudden loss of that bond places the body into a state of alarm, as though something essential to survival has disappeared.
This helps explain why grief can feel so physically distressing: the body is reacting to danger, not metaphor.
The Loneliness of Loss and the Brain’s Search
One of O’Connor’s central themes is the brain’s effort to make sense of absence. After a loss, the world can feel painfully unfamiliar. Widows and widowers often describe a deep loneliness that cannot be easily named—not merely the absence of companionship, but the absence of a shared reality.
O’Connor explains that grief is not just cognitive (“I know they are gone”), but also emotional and neurological. The brain continuously predicts where our loved one will be, how they will respond, and how we will move through the world together. After a death, the brain must repeatedly confront the mismatch between expectation and reality.
This ongoing process of recalibration is exhausting and can leave grieving individuals feeling confused, unfocused, or emotionally overwhelmed.
The Body Keeps the Score of Loss
A particularly sobering contribution of The Grieving Brain is O’Connor’s discussion of the physical risks associated with bereavement. Research shows that chronic health conditions may emerge or worsen sooner following the death of a loved one. The prolonged stress of grief can accelerate inflammation, weaken immune functioning, and exacerbate underlying medical vulnerabilities.
O’Connor highlights the well‑documented “widowhood effect,” which shows a significantly increased risk of illness and mortality following spousal loss. In the first one to three months after a wife’s death, a surviving husband’s risk of death approximately doubles. Following a husband’s death, a surviving wife’s risk increases by approximately 50 percent. While this elevated risk decreases over time, bereavement is clearly a period of heightened physical vulnerability.
In rare but real cases, sudden cardiac events—sometimes referred to as “broken heart syndrome”—can occur following acute emotional loss.
Clinical Implications and Compassionate Care
O’Connor’s work carries an important message for both clinicians and bereaved individuals: grief deserves medical and psychological attention. Survivors are often encouraged to “be strong” or “move on,” yet the science suggests the opposite—grief requires care, monitoring, and compassion.
Medical follow‑ups, mental health support, and reduced self‑criticism during early bereavement are not indulgent; they are protective. Understanding grief as a biological process may also relieve some of the shame grieving individuals feel when their bodies seem to “betray” them.
A Grounded, Hopeful Perspective
While The Grieving Brain is rooted in neuroscience, it is ultimately a deeply humane work. O’Connor does not offer quick solutions or timelines. Instead, she emphasizes that adaptation after loss takes time and that the brain is capable of relearning a world forever changed.
This book is particularly valuable for grief therapists, medical professionals, and anyone navigating loss. It validates the experience of grief as both profoundly painful and deeply human—something that happens not because we are weak, but because we are bonded.
Final Reflections
The Grieving Brain reframes grief as a biological, relational, and survival‑based experience. Mary‑Frances O’Connor reminds us that love does not end when someone dies—and neither does the body’s memory of that love.
Grief lives in the body because love lived there first.
Gaslighting: What It Really Means (And Why We Need to Stop Misusing It)
Have you ever heard someone say, “You’re gaslighting me!” during an argument? These days, the term pops up everywhere—social media, TV shows, even casual conversations. But here’s the thing: gaslighting isn’t just a trendy buzzword. It’s a serious form of psychological manipulation, and when we throw it around carelessly, we risk losing sight of what it really means.
Have you ever heard someone say, “You’re gaslighting me!” during an argument? These days, the term pops up everywhere—social media, TV shows, even casual conversations. But here’s the thing: gaslighting isn’t just a trendy buzzword. It’s a serious form of psychological manipulation, and when we throw it around carelessly, we risk losing sight of what it really means.
Let’s dive deeper into what gaslighting really is, why it’s harmful, how to spot it, and what to do if you’re experiencing it.
What Exactly Is Gaslighting?
Gaslighting is more than lying or disagreeing—it’s a deliberate, ongoing effort to make someone doubt their reality. The term comes from the classic film Gaslight, where a husband manipulates his wife into questioning her sanity by dimming the lights and denying it ever happened.
In real life, gaslighting looks like:
Intentional distortion of reality: “That never happened. You’re imagining things.”
Power imbalance: It often occurs in relationships where one person holds more control.
Long-term impact: Over time, the victim starts questioning their own memory and judgment.
Gaslighting is not a one-time lie or a heated argument. It’s a pattern of behavior designed to erode someone’s confidence in their own perception.
Why Is It So Harmful?
Gaslighting isn’t just frustrating—it’s damaging. Victims often experience:
Loss of self-trust: They stop believing their own thoughts and feelings.
Emotional dependence: The manipulator becomes the “truth-teller.”
Mental health struggles: Anxiety, depression, and trauma are common outcomes.
Imagine constantly second-guessing yourself—wondering if you’re “too sensitive” or “making things up.” That’s the reality for many people who experience gaslighting.
When We Misuse the Term
Here’s the problem: “gaslighting” has become shorthand for any disagreement or lie. That’s not accurate—and it matters. Misusing the term can:
Dilute its meaning: Real victims struggle to be heard when the word is overused.
Create confusion: Not every argument or misunderstanding is gaslighting.
Trivialize abuse: It’s a serious issue, not a casual insult.
Gaslighting requires intent and repetition. A single lie? Not gaslighting. A difference in opinion? Definitely not gaslighting.
How to Spot Gaslighting
If you’re wondering whether you’re experiencing gaslighting, look for these signs:
Repeated denial of facts you know to be true.
Twisting your words to make you feel irrational or “crazy.”
Minimizing your feelings (“You’re too sensitive” or “You’re imagining things”).
Rewriting history to fit their narrative.
Making you question your memory or judgment over time.
Creating dependency so you rely on them for “the truth.”
If these behaviors happen consistently and intentionally, it may be gaslighting—not just a disagreement.
What to Do If You’re Being Gaslighted
Recognizing gaslighting is the first step. Here’s what you can do:
Document what happens: Keep a journal of conversations and events.
Seek outside perspective: Talk to trusted friends or a therapist who can validate your experiences.
Set boundaries: Limit interactions with the person if possible.
Prioritize your mental health: Gaslighting can take a toll—professional support can help you rebuild confidence.
Know when to walk away: In severe cases, leaving the relationship or environment may be necessary for your well-being.
The Bottom Line
Gaslighting is a powerful term for a harmful behavior. Let’s use it carefully. When we understand what it truly means, we can better support those who experience it—and keep our conversations honest and respectful.
References
Abramson, K. (2014). Turning up the lights on gaslighting. Philosophical Perspectives, 28(1), 1–30.
Sweet, P. L. (2019). The sociology of gaslighting. American Sociological Review, 84(5), 851–875.
Sarkis, S. (2018). Gaslighting: Recognize Manipulative and Emotionally Abusive People—and Break Free. Da Capo Lifelong Books.
American Psychological Association. (2023). Gaslighting. APA Dictionary of Psychology. Retrieved from https://dictionary.apa.org/gaslighting